Part 1 Summary Conclusions
- Extensive data analysis does not support the media-induced hysteria
- The coronavirus for people under 65 has a fatality rate the same as commuting to work
- Undercount of cases means the virus is not as deadly as you think
- Nursing home and long-term care facilities account for nearly half of U.S. deaths
- Children have a 99.99% survival rate
- The virus is not as infectious as you think. Infection from surface transmission in question
- New York’s gross mishandling of the outbreak freaked out a nation
- The spread is primarily among Essential Services workers and their community and public transportation is the delivery mechanism
- There will likely NOT be a second wave
- Therapeutics are on the way
- There may already be a vaccine and it was invented in 1921
Series Introduction
Warner’s Corner is embarking on an ambitious multi-part series entitled “When Models Break”. Society, governments, healthcare, the economy and the financial markets are all based on models. Some are literal quantitative models, like epidemic curves, and some are more theoretical like forced lockdowns. Models govern the way we live. The coronavirus did not just attack human immune systems but the very underpinnings of society by causing many of the models on which society operates to bend and even break.
This series has three parts. Part 1 sets the record straight on what the coronavirus is, how it spread and the path forward as the economy re-opens. Part 2 will provide our view of the financial markets and what it means to inject trillions of dollars of stimulus. Part 3 will offer our thoughts on the upcoming election and its implications with regard to the economy and our engagement with the world.
Introduction
Since the outbreak became international news in January we have followed every twist and turn. From charting daily cases in various countries and states to reading dozens of epidemiological and medical studies every week, we hoped to gain an informational advantage and use this information to provide an investment edge. Importantly, we also hoped our knowledge may provide an antidote to fear. We could not have made a better decision.
We have given numerous interviews and video presentations, produced written reports, responded to emails and spent hours on phone calls during the last four months providing updates on our findings. There are many other work products that never saw publication as we developed and evaluated hypotheses and scoured medical studies, translated foreign websites and collected alternative data sets to search for evidence on topics ranging from the coronavirus’ spread, its real hospitalization rate, ventilator usage and mortality rate. We chased down rumors – often spread by major media outlets – and to our dismay have found more often than not mistruths and even outright deception as this virus has inexplicably become a political football.
Our research, while hopefully beneficial to calming fears, produced in us – stewards of wealth – an inner strength and calmness that enhanced our ability to navigate the ensuing market crisis, which was as unprecedented and violent in its swiftness as the virus itself. In times of crisis, “cooler heads” prevailed. We hesitated in writing a piece – that I promise comes shortly after this preface – that laid bare much of our analysis but we realized that there is still a large amount of fear in society stoked by the flames of mis/disinformation. So, we felt compelled to share our research results about the virus.
COVID-19: Setting the record straight
Over the course of the last five months, we have been asked the following questions:
- What is it?
- Where did it come from?
- How contagious is it?
- How deadly is it?
- Are my children at risk of dying?
- Do we have enough ventilators and hospital beds?
- Do we need more testing?
- How long does the virus last on a cardboard box?
These questions all have one thing in common: fear.
Understandably, most people have not made understanding this virus their full-time job and so they hear things but lack an overall ability to separate real information from misinformation and then put that information into an appropriate context.
We are standing on the shoulders of giants in the scientific and medical community as their tireless work under strenuous conditions produced a remarkable amount of statistically significant data. Allow me to introduce you to the virus without any bias. Just the truth.
The virus is a new coronavirus and in the same family as influenza. It has some characteristics that are similar and some that are not. We know it is particularly deadly for people with pre-existing conditions and the older the person the more deadly the combo. In Italy, we know that 84.8% of deaths were of persons aged 70 years or older1 and 59.8% of all deaths were patients with 3 or more pre-existing conditions2. Similar data can be found at health ministries all around the world. This is a dangerous virus for those who are older and battling other health problems.
Assumption: COVID-19 is a very deadly disease. FALSE
“…19.9% of all New York City residents had antibodies (1.65 million) further implying a fatality rate of just 1.0% NOT 8.4%”
There is nothing scientifically proven to confirm this assertion. The key problem with calculating mortality rates for any geography is we do not have an accurate count of cases. We surmised this was the case early on because we found a Chinese report that traced a case back to the middle of November 20193. The Chinese Government finally acknowledged the virus’ existence at the end of December. Whichever date you believe, there were 94 daily flights to 19 countries still operating out of Wuhan International Airport for weeks until travel bans were put in place and the airport was ultimately closed. The virus got out and multiplied globally. There are many anecdotal stories but we rely on data from New York State, which has been conducting extensive antibody tests on thousands of its citizens throughout the state. They have found that 12.3% of the general population has virus antibodies4. That means that 2.4 million New Yorkers have contracted the virus NOT 343k as reported. That also means that the fatality rate is 0.9% NOT the reported 6.5%! The study further implied (statistically significant) that an incredible 19.9% of all New York City residents have antibodies (1.65 million) further implying a fatality rate of just 1.0% NOT 8.4% using reported figures5.
Mass General Hospital also conducted an antibody study on Boston residents and found that 10% had antibodies implying 71k cases NOT 11k. Therefore, the fatality rate there is 0.78% NOT 4.8%.
Total Cases in these cities were 7-8x undercounted. The virus is simply not as deadly as you have been told.
The media has the propensity to twist the facts to generate more interest. Here’s an article from The Boston Globe reporting the MGH antibody test6. The title of the article is “Boston study in 4 areas finds 9 out of 10 people have not been exposed to coronavirus”. This strangely worded title buries the lead that 1 in 10 have already had it!
In fact, there have been quite a few antibody studies and population subgroup studies from various counties and cities around the world over the last few months, that concluded that the fatality rate of this coronavirus is just 0.2% globally7.
In other words, you are just as likely to die on your commute to work.Further, an additional global study found that the fatality risk for anyone under the age of 65 who contracts the virus is equivalent to the risk of death from driving between 13-101 miles8. In other words, you are just as likely to die on your commute to work.
“In other words, you are just as likely to die on your commute to work.”
The Tragedy of Nursing Home Deaths
Easily the most tragic aspect of this pandemic is how U.S. states to varying degrees completely failed to protect the most vulnerable of society: our sick and elderly in nursing homes and long term care facilities. There was clear evidence from China, Korea, Italy, Spain and all the countries that dealt with the coronavirus before it hit the U.S., that the elderly and especially those with pre-existing conditions were at extreme risk. The preferred method of prevention was to prevent visitors and family from these facilities but this was clearly not enough as infected Essential Services workers brought in the infection or worse yet certain states, including New York, Massachusetts, New Jersey and California, actually transferred positive coronavirus patients into some of these facilities9.
The extraordinary poor strategies employed for protecting our most fragile has led the death count in the U.S. The common refrain we hear from the media is that one-third of all U.S. deaths are associated with nursing homes10. This is hard to verify. One of the problems we have is just getting to an accurate count. Despite each state being required to disclose these fatalities to the CDC, the nursing homes are not required to share this information publicly. So, nursing homes in over a dozen states are withholding this information, according to the AARP. On April 19th, the Centers for Medicare & Medicaid Services (“CMS”) issued an order for nursing homes to report deaths directly to the CDC to fix this problem11. CMS Administrator Seema Verma subsequently ordered that this reporting obligation would commence no later than May 17th12. The CDC has yet to disclose any figures.
Nevertheless, independent researcher Phil Kerpen has been tracking deaths on a bottoms-up basis state-by-state and via media reports and has determined that approximately 42,917 deaths from the virus were residents of a nursing home or long-term care facility13. This would mean that 45% of virus deaths in the U.S. were in these facilities. His analysis further found that there have been 185,735 virus cases in such facilities therefore implying a fatality rate of 23.1%.
Ergo, only 50,641 deaths have occurred outside nursing homes in the U.S.
As sad at this subject of deaths at nursing facilities is, even this needs to be put into perspective. Of the over 5 million Americans that live in long-term care facilities, the CDC says that 380,000 die every year from infections, including urinary tract infection, diarrheal disease, antibiotic-resistant staph infections and many others.14
Assumption: Aren’t Children at Risk of Dying? FALSE
The media would lead people to believe that many children are dying from the coronavirus, however, this is untrue. Here are some facts. There have been over 36,000 cases among children under 18 years old in the U.S.15.
- Survival rate is 99.99% - Per the CDC, as of 5/20/20 only 12 children under the age of 15 have died with COVID-19 in the U.S.16
- Hospitalization rate nearly zero - Per the CDC, the hospitalization rate among American children aged 0-4 with COVID-19 is 0.003% and 0.001% for ages 5-17. In terms of actual numbers, there have been 58 total hospitalizations among 0-4 year olds with the virus and 74 for ages 5-1717
- Pre-existing conditions are a key driver - Per a JAMA study, there were 48 children admitted to pediatric ICUs from March 14 to April 3, 83% of whom had an underlying condition. The primary comorbidities were: Developmental delay/genetic anomalies, immune suppression, obesity and diabetes. The fatality rate of these patients was 5% compared to 50-62% for adults.18
- Potentially at lower risk of infection – A recent antibody study conducted by the Instituto de Salud Carlos III in Spain, found that antibodies were present in just 1.1% of infants under 1 year old, 2.2% in 1-4 year olds, 3.0% in 5-9 year olds, 3.9% in 10-14 year olds and 3.8% in 15-19 year olds versus the country average of 5.0%.19
- Potentially not significant spreaders – According to a study of infections in school children and staff by the Australian National Centre for Immunisation Research and Surveillance, it suggests that children are not significant spreaders of the cororonavirus20. In early March, a total of 18 positive cases were found in 10 New South Wales high schools and 5 primary schools. The cases were equally split between students and staff. The public health staff investigated 863 close contacts and only two students were identified as secondary cases. Notably, one transmission was student-to-student, there was no transmission from student to staff and one transmission of staff-to-student.
It is evident that children react differently to the coronavirus than adults. The risks of severity, mortality, susceptibility, and ability to transmit the virus to others is seemingly very low. Even much lower than that of the seasonal flu.21
Assumption: COVID-19 is a very infectious disease.
In science, the speed of infection is known as the reproduction rate (R). This is a measure of the number of other people infected by an infected person. There is no statistically conclusive data we can find today on this virus’ infectiousness. This calculation by its nature is very difficult to accurately capture. One of the best studies we found looked at the R values of previous pandemics, including the influenza pandemics of 1918 (aka the Spanish flu), 1957, 1968 and 2009 as well as six novel corona virus outbreaks, including MERS and SARS22. Of the 111 studies reviewed, the mean R values ranged from 1.46-1.80 from the flus and <1 for the novel corona viruses. The seasonal flu has a median R of 1.28 by contrast. But to repeat we do not know what the R is of this virus, but it wouldn’t be irrational to think it is similar to other coronaviruses. We just don’t know.
For comparison purposes, the 2018-2019 flu season was a relatively bad one. The CDC estimates that up to 37.4-42.9 million people got sick23. That’s 11-13% of the entire US population and that’s with 49% of the population being vaccinated24. Prior to this crisis, it never dawned on me (and likely most Americans) just how infectious the seasonal flu is. Would the coronavirus have ultimately infected over 40 million had lockdowns not been implemented? Possibly? But here again, we have very conflicting data as we look around the world. Sweden didn’t execute full lockdowns and has had just over 30k cases25, representing just 0.3% of the population.
Further, the more we know about this virus less contagious it gets. On 5/21/20, the CDC revised its view of the ability to be infected from touching surfaces or objects.
Old Guidance: “It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their mouth, nose or possibly their eyes.”26
New Guidance: “The virus does not spread easily in other ways…From touching surfaces or objects. It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their mouth, nose or possibly their eyes. This is not thought to be the main way the virus spreads, but we are still learning more about this virus.”27
The more we learn about the virus the less fatal, less infectious and the less relevant to under 65 year olds not in nursing homes. The data could not be more clear.
The New York Experience and its Impact on the Nation
In hindsight, it seems inevitable that our largest city with millions of commuters coming and going every day and thousands of international travelers entering via two of the busiest international airports in the world, that a pandemic would hit New York City (and the Tri-State area) hard. Given the novel nature of this virus and critical early epidemic modeling errors, the city was griped with hysterical fear. As home to the major media outlets, the nation has been glued to their nightly news reports and news apps. And, as news programs are wont to do, stories about the potential lack of ventilators, hospital beds, PPE, masks along with the Navy Hospital ship “Comfort” pulling into port flooded the airwaves. Governor Cuomo and Mayor DeBlasio cited poorly constructed epidemic models by McKinsey and the CDC that showed that 80% of New Yorkers would become infected and that 30-40k ventilators would be needed28 – 10x more than they had. Justifiably so, not just New Yorkers but the entire country was engulfed in fear as these stories fed anxiety over a deadly virus with no cure.
As time has passed and the outbreak has become largely contained, researchers have begun to look more closely at how and why the virus spread so quickly in New York City. Recall from above that 20% of New York City residents have already had the virus and nearly all recovered, according to antibody studies conducted by the state. While many have simply deemed that the outbreak was due to population density, that characteristic alone does not fully explain why its experience was so much worse than other even more densely populated global cities.
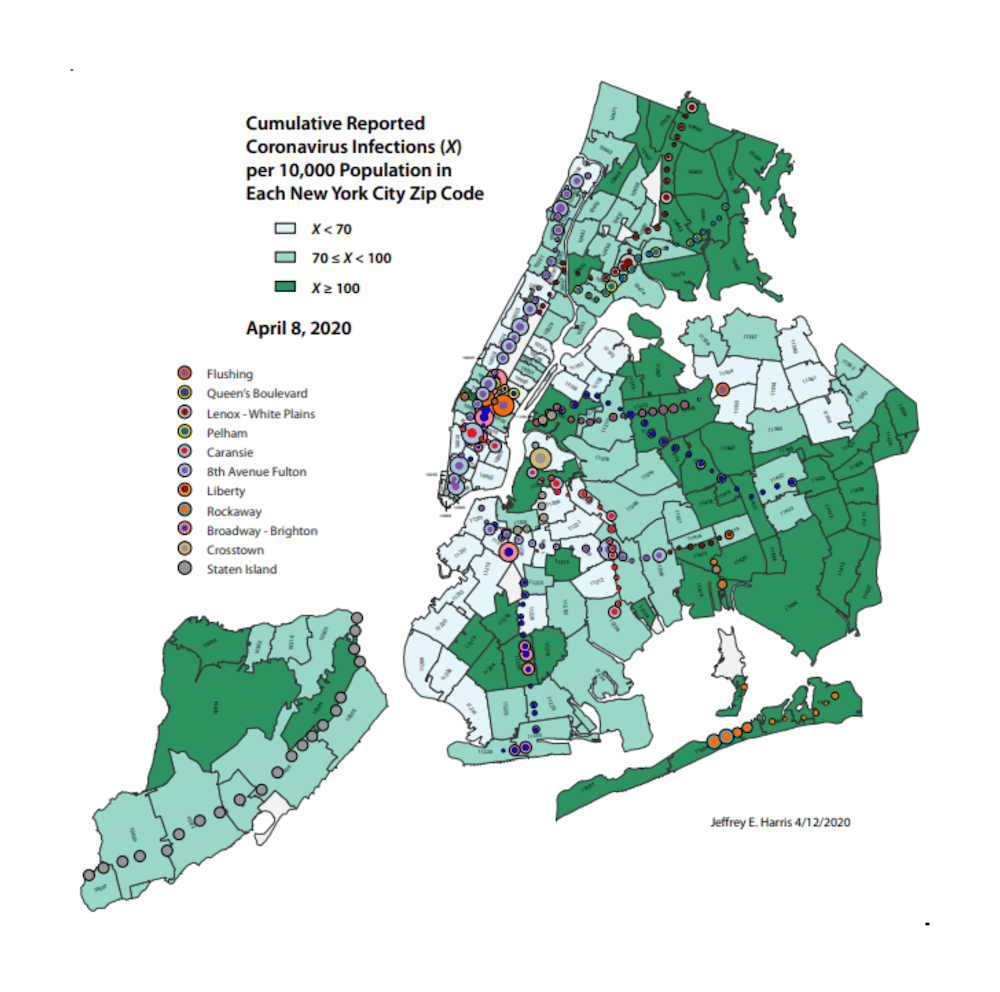
MIT Economics professor, Jeffrey Harris recently published an intriguing study on how the virus spread in New York City29. He took the map of the confirmed cases by zip code and overlay the NYC subway map. One particular Queens zip code was especially hard hit by March 31st as most other zip codes had relatively few cases. Just 8 days later the surrounding zip codes were equally as infected and the high case numbers had spread to the Bronx, Brooklyn and Staten Island.
Professor Harris found that the zip codes with the heaviest cases lay along the major commuting subway lines with the first clustering around the Flushing Local Line stations. The Flushing line connected this highly infected Queens zip code through Long Island City and into West Midtown Manhattan (the Times Square area). He relies on two other studies to assert that the workers commuting into Manhattan were lower-paid, Essential Services workers. As the lockdowns began, these workers were required to continue to commute in while Manhattan residents, who are largely white collar, sheltered-in-place. Cases leveled off in Manhattan, yet cases in the other lower income boroughs continued to increase.
“…these trains were not cleaned and disinfected on a daily basis”
Professor Harris also cites two specific decisions made by Mayor DeBlasio that dramatically worsened the outbreak. First, with the lockdown in place for non-Essential Services workers and an associated 65% drop in ridership, he reduced the number of trains running by two-thirds to save money. By doing so, however, he forced these Essential Services workers to board crowded trains during their commute. Second, he eliminated Express lines as part of this cost saving effort but by doing so it increased the time to commute and permitted the entry of potentially infected persons at every local stop thereby increasing the risk of infection to all riders. And then to top it off, these trains were not cleaned and disinfected on a daily basis30. Effective daily cleaning did not start until nearly two months after the first reported case. It was poor decision-making that contributed to the outbreak’s acceleration.
Two important realizations come from this study. First, a disproportionately high number of cases are among Essential Services workers. People that were required to continue working. Second, New York City failed to protect the oldest and most vulnerable among these workers. For instance, 22% of NYC Metropolitan Transportation Authority employees are 55 years or older31. That’s nearly 15,000 people that probably should have sheltered-in-place.
The New York experience was indeed grossly mishandled and will likely be studied for years to come but not before many lives were needlessly lost. Nevertheless, the major news outlets never reported on these critical drivers of the outbreak but rather created hysteria by focusing on the WHAT not the HOW or WHY. This fear spread to every corner of the country even as local and regional experiences differed vastly.
The Dallas County Experience
We sought to leverage these learnings and apply them to Dallas County. We took the map of Dallas County coronavirus cases by zip code and overlay the DART Commuter Rail station map. There was a correlation. But we also learned something else. Virus cases are much more prevalent in low income zip codes and those are overwhelmingly Hispanic in Dallas County, which we verified through several different real estate websites.
It seems that one of the cruelest aspects of this virus has been not just its disproportionate effect on the elderly but its impact on Hispanic and African-American populations. We hypothesize that these workers, like those in Queens, are disproportionately commuting via public transportation to Essential Services jobs and, therefore, have not been required to shelter-in-place. The US Bureau of Labor Statistics in 2015 published a report looking more specifically at Hispanic workers and found the highest proportion of Hispanic workers in Construction, Agriculture, Leisure and hospitality and other services32. These were deemed essential during the Dallas County lockdown.
We believe but have yet to verify that tied to the spread of the virus is the willingness of sick workers to stay at home. For white collar workers, this is a relatively easy decision but not so for those employed illegally or for those employed by companies that do not provide paid sick leave. According the US Bureau of Labor Statistics’ March 2019 “National Compensation Survey” on employee benefits, 24% of US workers do not receive paid sick leave33. These jobs are predominantly in the lowest deciles of average wages paid.
A critical question emerges, how does society create the right incentives so that the most economically fragile workers and those who need to work the most, forego badly needed income and stay home when they are sick? It is fundamentally contrary to 24% of American workers’ most pressing needs to stay-at-home. They don’t have a choice unless one is created.
It is this finding that translates city after city. San Francisco, Boston, Chicago, New Orleans, Detroit, Philadelphia, DC, for example, all show the worst outbreak of cases in their low income zip codes. It would seem to us that cities really failed to recognize where this virus exists, how to stop it from spreading (e.g., better subway management) and protecting those most at risk.
The Most Gating Question: Will We Have a Second Wave?
Which brings me to perhaps the most important question we face as a society today. Will we have a second wave of the coronavirus? The answer to us seems to be most likely “No” for several reasons. Could we see clusters of cases here and there? Yes. But we don’t expect a large outbreak. Here’s why.
- “We” don’t have it. We tend to forget that if we have all been in quarantine for months, we don’t (still) have the virus. But when I say “we”, I am talking about white collar, Non-Essential Services employees, students and retired persons. That “we” has very little to fear as “we” begin to comingle. The media has scared people into thinking that “we” could all just be asymptomatic. No medical evidence supports a period of contagiousness anywhere close the extent of the lockdowns. “We” don’t need to be tested to know that “we” are virus free.
- The re-openings are going very slowly. The slow motion re-openings of states is also helping to contain any further large outbreak. For example, on Monday 5/18/20 office workers were permitted to return to their offices in Texas. We’ve been in the office for 4 weeks and, frankly, enjoy the easy commute these days. But it appears very few have come back to their office. A rough survey of companies we follow shows a very slow and deliberate return. Many offices need to be reconfigured to account for Social Distancing policies and those policies themselves are still under development. Some businesses may require testing for employees to return. Our impression is that current sentiment is to proceed slowly and that will help stave off a rash of new cases. In fact, Facebook, large New York banks and other companies are considering more permanent remote working solutions.
- Increased testing of Essential Services workers. With the Non-Essential Services workers in lockdown, the virus is circulating primarily among Essential Services workers. In Dallas County, for instance, 80% of all hospitalizations are Essential Services workers and their immediate families34. On April 20th, the county implemented free testing to any Essential Services worker and residents over the age of 65 with a pre-existing condition whether they have symptoms or not. Many doctors’ offices and hospitals have now implemented weekly and sometimes daily testing of their employees. It is critical that these at-risk workers, particularly those in hospital environments, not be allowed to transmit the virus to co-workers, family members and, especially, nursing home patients. Testing strategies like this are being implemented elsewhere.
- Higher self-awareness. Human beings learn from experience and we have all learned various new behaviors, such as hygiene strategies, wearing masks, standing 6 ft apart, etc. Four months ago, we were oblivious to all of this. Now we have hand sanitizer everywhere. The virus has an uphill battle even if we just continue to do these simple things.
- Better prevention tactics. Businesses are cleaning more often. Public transportation officials have adopted daily cleanings of their buses and trains at a minimum. In our office building, foot operated door openers have been placed on restroom doors and the sink is donned with signs on how to wash your hands and even offers up a list of songs you can hum to let you know when to stop.
- “We” have more testing. Let’s clear one thing up. Testing is no panacea. Testing is like the Balance Sheet of a company. It reflects one point in time only. You could take a test and be negative and the next day contract the virus. However, testing does create some peace of mind. This is particularly important as we think about opening schools. I spent considerable time above debunking how dangerous this virus is to children but let’s go ahead and test all the kids and teachers just before they go back to school. Peace of mind.
Quick Word on Therapeutics & Vaccines
According to the Milken Institute, which has a great tracker35, there are currently 218 therapeutics (treatments) and 140 vaccines currently under development. The sheer number reflects the astonishing global scientific effort underway.
The very first new therapeutic, Remdesivir, has been expedited for patient use and may be successful in shortening recovery times. Others are on the cusp of being greenlighted. The goal of therapeutics is to help prevent mild cases from becoming severe and severe cases from becoming lethal. We won’t go into all the different ways each therapeutic is attacking this problem but the early results look promising and immediate. Hydroxychloroquine, a commonly used malaria therapeutic, has received notoriety over the last few weeks as President Trump touted it (and is even taking it now) even as the CDC has not blessed its usage on COVID-19 patients. There have been several inconclusive studies thus far in different countries. But we are not ready to completely dismiss it – as major media outlets have – until we see the results from a University of Washington study due in July. This study has sufficient patient numbers to generate statistically significant results.
On the vaccine front, there is still a long way to go. Most vaccine efforts are still early and not even in Phase 1 trials. The furthest along seem to be the Inovio, Moderna and AstraZeneca vaccines which are in Phase 2. Although proceeding at record pace and global governments streamlining approval processes, the process of getting a drug approved that will be safe for 8 billion people to use is daunting and time consuming and probably a year in the making.
A much faster process would be if we already had a vaccine on the shelf for another disease that could be repurposed. As virus case data has been collected globally, many observers have begun to wonder why certain countries have reported much fewer cases and better outcomes, such as Korea, India, China and parts of Africa. There is a study underway by the Murdoch Institute in Australia to determine if a common universal tuberculosis vaccine (Bacillus Calmette-Geurin or “BCG”) is providing protection against the coronavirus. It was introduced in 1921. A recent study from the New York Institute of Technology36 offers some supportive evidence. This drug is offered in many countries, but not in the US or most of Western Europe, largely because tuberculosis ceased to be a major health risk decades ago. For example, Spain does not require BCG vaccination and had over 230,000 cases but its next-door neighbor Portugal, which does universally vaccinate, had just 30,000. We’ll know soon enough as the Australian trials should conclude by Christmas and there may be some indicative conclusions by the end of October37.
We are a big believer in human ingenuity and fortitude. With so many great treatments on the way and let’s not forget the incredible body of knowledge that grows by the day in how best to treat the most sick, the medical community has increasingly more powerful tools to save the most at risk and prevent disease escalation. That alone should provide sufficient comfort for most people to resume their lives without fear. A vaccine, in our opinion, is the cherry on top.
Conclusion
Studies performed by the scientific medical community refute the infectiousness and severity of the coronavirus that is asserted by media outlets. The disconnect between the truth as these studies assert and the misinformation we hear through major news outlets is phenomenal. We would be remiss if we heaped all of the blame on just the major news networks because we hear similar misleading statements from political leaders on both sides of the aisle and even Dr. Faucci himself38. As we have observed during the last four months, this misinformation created hysteria. Now, we have data on our side and it is time to let it govern our actions and emotions.
One of the most extraordinary findings is the role that public transportation played in spreading the outbreak in New York City. Learning from that and the many other strategies that have been developed will let this economy re-open without a second wave. My sincere concern is that when this chapter of history is written the virus itself will be a footnote to the real social and economic damage that these lockdowns created.
Let me conclude by saying enough is enough with the misinformation from the media. Thanks for reading.
Part 2 will reflect on the social and economic damage, the fixes that are being applied and what that all means for financial markets. Stay tuned.
Jim Warner is the Managing Director, Head of Research of Lear Investment Management. Lear is an investment firm founded in 2015 focused on generating returns with measured risk. With a quarter century of experience, his ability to identify attractive investment ideas, construct portfolios and manage risk has resulted in superior outcomes for clients.
The Lear Global Vigilance Strategy is rated 4 Stars by Morningstar and ranks in the top 12% of managers in the Tactical Allocation category.
1https://www.epicentro.iss.it/en/coronavirus/bollettino/Infografica_18maggio%2520ENG.pdf
2https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_14_May_2020.pdf
3https://www.scmp.com/news/china/society/article/3074991/coronavirus-chinas-first-confirmed-covid-19-case-traced-back
4https://www.governor.ny.gov/news/video-audio-photos-rush-transcript-amid-ongoing-covid-19-pandemic-governor-cuomo-announces-17
5https://www1.nyc.gov/site/doh/covid/covid-19-data.page
6https://www.bostonglobe.com/2020/05/15/metro/boston-study-4-areas-finds-9-out-10-people-have-not-been-exposed-coronavirus/
7https://swprs.org/studies-on-covid-19-lethality/
8https://www.medrxiv.org/content/10.1101/2020.04.05.20054361v2
9https://www.aarp.org/caregiving/health/info-2020/coronavirus-transfers-to-nursing-homes.html
10https://www.nytimes.com/interactive/2020/05/09/us/coronavirus-cases-nursing-homes-us.html
11https://www.cms.gov/files/document/qso-20-26-nh.pdf
12https://www.aarp.org/caregiving/health/info-2020/nursing-homes-to-publicly-disclose-coronavirus.html
13https://docs.google.com/spreadsheets/d/1ETm51GayRjlnoaRVtUOWfkolEeAQZ-zPhXkCbVe4_ik/edit#gid=435667374
14https://www.cdc.gov/longtermcare/index.html
15https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
16https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-W/vsak-wrfu
17https://gis.cdc.gov/grasp/COVIDNet/COVID19_5.html
18https://jamanetwork.com/journals/jamapediatrics/fullarticle/2766037
19https://www.lamoncloa.gob.es/serviciosdeprensa/notasprensa/sanidad14/Documents/2020/130520-ENE-COVID_Informe1.pdf
20http://ncirs.org.au/sites/default/files/2020-04/NCIRS%20NSW%20Schools%20COVID_Summary_FINAL%20public_26%20April%202020.pdf
21https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
22https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4169819/
23https://www.cdc.gov/mmwr/volumes/68/wr/mm6824a3.htm?s_cid=mm6824a3_w
24https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm
25https://experience.arcgis.com/experience/09f821667ce64bf7be6f9f87457ed9aa
26https://web.archive.org/web/20200328203140/https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html
27https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Ftransmission.html
28https://www.syracuse.com/coronavirus/2020/03/cuomo-refutes-trump-insists-ny-needs-up-to-40000-ventilators-i-operate-on-facts.html
29 “The Subways Seeded the Massive Coronavirus Epidemic in New York City”, Jeffrey E. Harris, MIT, April 24.2020
30https://nypost.com/2020/04/30/nyc-subways-will-close-overnight-for-coronavirus-cleanings/
31http://www.nyc.gov/html/sbs/wib/downloads/pdf/urban_transit.pdf
32https://www.bls.gov/opub/ted/2015/hispanics-and-latinos-in-industries-and-occupations.htm
33https://www.bls.gov/ncs/ebs/benefits/2019/ownership/private/table45a.pdf
34https://www.dallascounty.org/Assets/uploads/docs/hhs/2019-nCoV/COVID-19%20DCHHS%20Summary_051920.pdf
35https://docs.google.com/spreadsheets/d/16DbPhF9OD0MHHtCR12of6yUcfiRzP_-XGkynEbnipds/edit#gid=2075421071
36https://www.medrxiv.org/content/10.1101/2020.03.24.20042937v1.full.pdf
37https://clinicaltrials.gov/ct2/show/NCT04327206
38https://dailycaller.com/2020/03/29/anthony-fauci-coronavirus-death-toll-prediction-america/
INFORMATION PRESENTED IS FOR EDUCATIONAL PURPOSES ONLY AND DOES NOT INTEND TO MAKE AN OFFER OR SOLICITATION FOR THE SALE OR PURCHASE OF ANY SPECIFIC SECURITIES, INVESTMENTS OR INVESTMENT STRATEGIES. INVESTMENTS INVOLVE RISK AND ARE NOT GUARANTEED. PAST PERFORMANCE IS NOT INDICATIVE OF FUTURE RETURNS. BE SURE TO FIRST CONSULT WITH A QUALIFIED FINANCIAL ADVISER AND/OR TAX PROFESSIONAL BEFORE IMPLEMENTING ANY STRATEGY DISCUSSED HEREIN.